Knee Osteoarthritis
One quarter of 50 year olds have knee pain and half of the 80 year old population have significant knee pain.
What helps?
- Exercise: pain free aerobic and resistance exercise is the scientifically proven intervention for improving knee osteoarthritis pain and activity levels.
- Aquatic or water exercise
- Hands on physiotherapy
- Losing weight
- Other interventions have limited evidence of improving knee osteoarthritis. These include: ‘offloading’ knee taping, orthotics, knee braces, altering your walking pattern
Physiotherapy (stretching and joint mobilising) has mild benefit in treating knee osteoarthritis. Manual hands on therapy in addition to prescribed exercises provides the best results, scientifically demonstrated to be better than performing exercises alone (Jansen, J. Physiotherapy, 2011).
Pool exercises do not appear to provide long term benefit. Yet, if you enjoy swimming or water based exercise, there is scientific evidence supporting this form of exercise for knee osteoarthritis.
Each of these interventions can be discussed and appropriately prescribed by our experienced physiotherapists at Richmond Physiotherapy Clinic.
Exercise
The most researched intervention for knee osteoarthritis is exercise – there are benefits for osteoarthritis from most types of exercise. Strengthening exercise includes resistance exercises, aerobic exercise, tai-chi, hydrotherapy or water exercises and home-based exercises. These involve exercises to improve hip strength with particular exercise on the gluteals.
Supervised exercises programs in addition to hands on physiotherapy result in substantially better outcomes. This involves regular progressions or modifications provided by a well experienced, post graduate educated physiotherapists at Richmond Physiotherapy Clinic.
Physiotherapy sessions provide improved long term pain relief, activity levels and strength, rather than doing exercises on your own (Mazières J. Bone Spine, 2008).
Losing weight
Losing weight improves knee osteo arthritis – 2 to 3 times body weight passes through the knee on each stride. The most proven way to lose weight is a combination of diet and exercise.
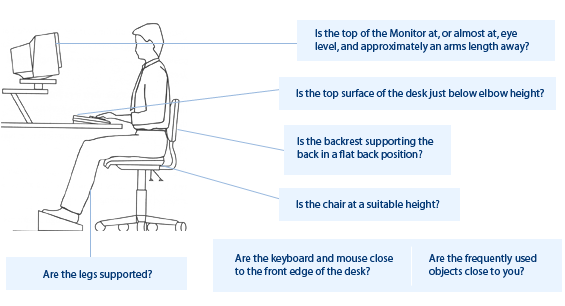
Changing the way you walk
Gait re-education training (changing the way you walk) appears beneficial to improve pain and function in knee osteoarthritis (Simic, J Biomechanics 2011). Using a walking stick reduces the knee joint load with a corresponding reduction in pain associated with walking. Please consult your Richmond Physiotherapy Clinic physiotherapist to demonstrate how to alter your walking with the view to reducing the load through the knee.
Medication
Whilst analgesics and anti-inflammatory medication appear to help, exercises are at least as beneficial and don’t have side effects. The physiotherapists at Richmond Physiotherapy Clinic attempt to find exercise that is enjoyable, ensuring the program is more likely to be sustained as an ongoing intervention and management strategy for knee osteoarthritis which, at the current time, does not have a cure.
Glucosamine sulphate
Glucosamine sulphate is a nutraceutical (not strictly a pharmaceutical) with mild beneficial evidence based support.
Misaligned knees
Misaligned knees (knocked knees or bow legs) do not improve as quickly in improving pain and strength than knees that have more normal anatomical alignment.
Braces and taping
Discuss with your physiotherapist whether it is worth trialling the various unloading tape techniques for the knee, with the view to reduce pain associated with physical activity. Many studies have examined braces and taping including neoprene sleeves and patella braces without any substantial proven benefit. The consensus opinion in the physiotherapy and medical world is if bracing or tape reduces your pain and allows you to perform activity with less pain, then it is ok to use them. The larger unloading braces tend to be bulky and uncomfortable and may cause skin irritation. There are also reports of DVT associated with larger braces plus they are difficult to fit with large overweight legs.
Orthotics
Orthotic wedges and various types of footwear do not have strong scientific evidence. However there appears to be some benefits in different footwear to increase pain free activity.
Does different footwear result in your knee giving you less pain with running, walking or playing sport? If so, then see your physiotherapist at Richmond Physiotherapy Clinic for bio-mechanical analysis to ascertain the contributing factors relating to your knee osteoarthritic symptoms.
Marathon long distance training
Does long distance running lead to knee osteoarthritis in the longer term? The evidence suggests in the absence of previous knee injury, there is no increased incidence of knee arthritis compared to the non-long distance running population. If you have had a knee reconstruction or knee surgery, including meniscus surgery, there appears to be an increased propensity to develop knee osteoarthritis with long distance running.
The information contained in this site is not intended as a substitute for advice from a qualified health care professional. Always obtain advice from a qualified health care professional before starting any exercise, stretching or health care program. The author and everyone involved in the production of this site disclaim any liability for any adverse effects resulting from the use of the information presented.